Over the last year, at least 17,000 health workers have died from COVID-19. A July 2020 investigation found that workers in 63 countries faced shortages of personal protective equipment (PPE) even as they treated COVID-19 patients. These shortages combined with the inequitable distribution of COVID-19 vaccines—low-income countries have vaccinated 1.9% of their populations—means that health workers in low-income countries face greater risk of infection and death than those in high-income countries.
“This pandemic has not really been easy for health workers in our city [Mbarara, Uganda],” Stephen Asiimwe, MBChB, MS, DrPH, Program Director of the Mbarara University of Science and Technology (MUST) Global Health Collaborative (GHC), says. “It has strained the health sector significantly, even reducing the healthcare workers that would be attending to other issues. And there are other effects we are beginning to learn from health workers: their children not going to school, others losing loved ones, and even some of us who have lost very close colleagues.”

Our thoughts continue to be with the families of Carol Orishaba (left) and Moses Ndema (right)
In July 2021, Carol Orishaba, RN, a nurse at Mbarara Regional Referral Hospital (MRRH) passed away after an extended battle with COVID-19. Less than a week later, Dr. Moses Ndema, a clinician in training at MRRH, passed away from the virus as well. Over the past three months our staff—both in Mbarara and Boston—have mourned these loses.
Orishaba was a 15-year veteran of MRRH and Mbarara University of Science and Technology (MUST). She practiced as a nurse in a clinical capacity at the hospital and also worked on several trials and research programs, including a landmark PrEP study and with MGH Global Health Research Collaborative member Mark Siedner, MD, MPH, on a cardiovascular research study. Described as a team player, Orishaba was a vital member of both clinical and research operations in Mbarara.
Ndema was a newer member of the MRRH and MUST community. He was a clinician in training, tirelessly offering himself in clinical settings where staff was needed. He was a clinical officer and recipient of a MGH Center for Global Health (CGH) First Mile scholarship which provided him the financial support to train and practice medicine. His death shocked and disheartened the community that he had dedicated his young career to serving.
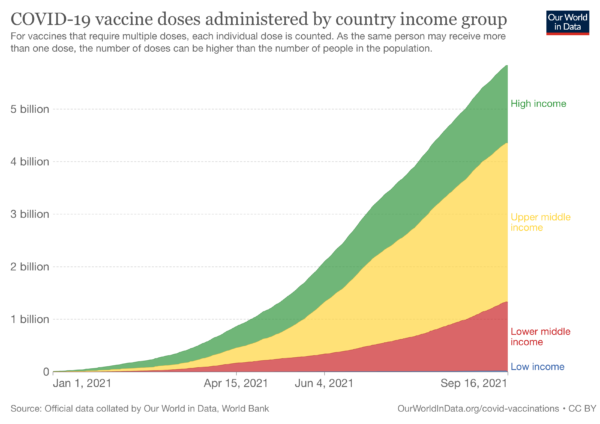
Both of these deaths came amid a COVID-19 second wave that struck Uganda, and other countries on the African continent. Uganda’s COVID-19 case count surged from May to June. On June 13, the country reported 2,800% more COVID-19 cases than it did on May 13. This third wave peaked on July 5, when the country reported 855 confirmed deaths and a 7-day average of 144 deaths. The rise in cases came after over a year of diligently working to control COVID-19. Though initial measures such as lockdowns and social distancing stalled the spread of the virus, numbers began to rise globally. At that time countries in the global north began to institute mass vaccine campaigns, while many others struggled to procure vaccines, leading to sharp increases in virus cases and deaths and a demand for greater global vaccine equity.
“The first thing is to increase advocacy for access to vaccines,” Asiimwe explains. “Then the second part is more personal protective equipment. Then training in the new protocols of how best to manage COVID-19. And finally, continuous medical education and updates on COVID research to counter the negative infodemic that came with the pandemic.”
In February 2021, members of the CGH community penned an open letter to US President Joe Biden and leaders of pharmaceutical industry calling for global vaccine equity. However, seven months later, the distribution of vaccines has continued to be unequitable: with projections that many low-income countries will not reach substantial vaccination levels until 2023.
“We miss [Orishaba and Ndema] so much,” Asiimwe says. “We don’t want to get a third wave because you never know who it will affect. And at this stage, where our vaccination rates are less than 2% nationwide, we can’t risk having another wave hit us. Most likely health workers will be the ones affected.”

